Advancements in Treating Philadelphia Chromosome-Positive ALL
In the treatment of newly diagnosed Philadelphia chromosome-positive acute lymphoblastic leukemia (Ph+ ALL), patients can experience significant improvements in their health outcomes, thanks in large part to the introduction of advanced therapies like the third-generation tyrosine kinase inhibitor (TKI), ponatinib. Recent research demonstrates that even if patients do not initially achieve a molecular response to ponatinib following their induction therapy, they still have a strong possibility of achieving minimal residual disease (MRD) negativity, markedly surpassing the statistics previous established with older TKIs such as imatinib.
A Study That Speaks to Improved Patient Outcomes
At the recent American Society of Clinical Oncology (ASCO) Annual Meeting, Dr. Ibrahim Aldoss from City of Hope hospital presented findings which emphasized the clinical benefits of continuing treatment with ponatinib beyond the third cycle in patients failing to achieve MRD negativity by the end of induction. The study documented a striking difference in outcomes, with 48% of patients continuing with ponatinib achieving MRD negativity by the fourth cycle, compared to only 33% for those on imatinib.
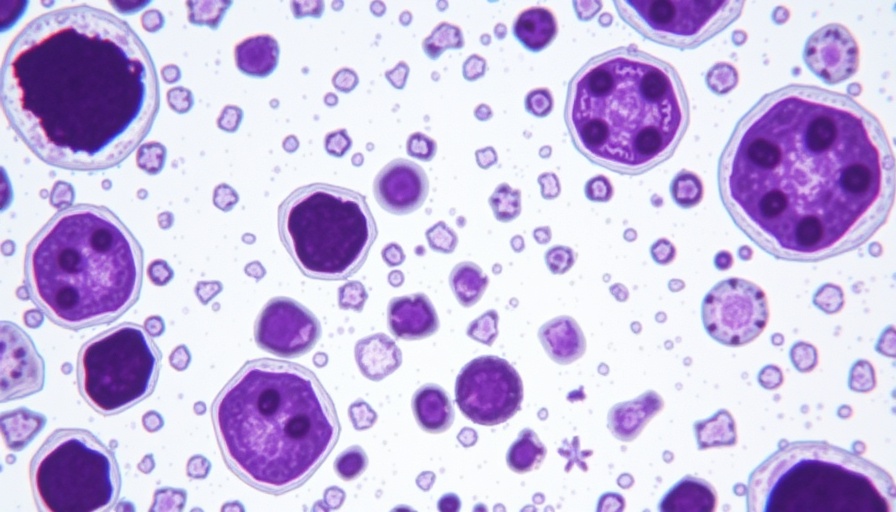
Understanding the Mechanics: How Ponatinib Works
Ponatinib is specifically designed to combat challenges posed by BCR-ABL1 variants including the T315I mutation, a significant hurdle in treatment. This targeted inhibition means that patients have a greater chance of achieving a complete molecular response, which correlates strongly with long-term survival rates. Earlier generations of TKIs simply could not address these complex mutations effectively, often leaving healthcare providers with limited options.
Potential Beyond the Initial Treatment: The Significance of MRD Negativity
Achieving MRD negativity is fundamental in managing Ph+ ALL. It reflects the absence of detectable leukemic cells, which is crucial for patients aiming for remission and long-term survival. In this recent analysis of 113 patients, those treated with ponatinib showed not only higher rates of MRD negativity but also were able to maintain this response significantly longer compared to imatinib group participants.
Event-Free Survival: A Closer Look at the Numbers
The statistics are telling: among those who did not reach MRD negativity after induction, ponatinib therapy had an event-free survival rate still rising, compared to 24.8 months for imatinib. With 82% of patients on ponatinib achieving event-free survival at two years versus 62% on imatinib, these figures powerfully highlight the drug's potential to change lives for those battling Ph+ ALL.
Side Effects and Considerations
While navigating through treatment options, it is also essential to understand the treatment-emergent adverse events (TEAEs). The research indicated that both treatments had similar side effect profiles, but with 100% of ponatinib patients experiencing side effects compared to 98% of those on imatinib, healthcare providers must remain attentive to patient experiences and adapt treatment accordingly.
Conclusion: A Growing Hope in Oncological Treatment
This study reinforces the message that continuous innovation in oncology can yield fruitful results. With proper guidance and treatment, patients diagnosed with Ph+ ALL can find new avenues of hope and more substantial, supportive care through TKI therapies like ponatinib. The journey of each patient can be further uplifted with ongoing support and informed dialogues about their treatment paths.
If you are or know someone navigating a diagnosis of Ph+ ALL, this progressive data is essential in advocating for the most effective treatments available. Embrace the advancements in medical research and make informed decisions regarding health and wellness.
 Add Row
Add Row  Add
Add 


 Add Row
Add Row  Add
Add 

Write A Comment