Breaking News: New Recommendations Change the Game for Gastric Cancer Prevention
Recently released guidelines from the American Gastroenterological Association (AGA) signal an urgent shift in how we approach gastric cancer prevention, particularly for high-risk groups. By advocating for rigorous endoscopic screening and surveillance of precancerous conditions, these new recommendations could dramatically reduce the incidence and mortality rates associated with this devastating disease.
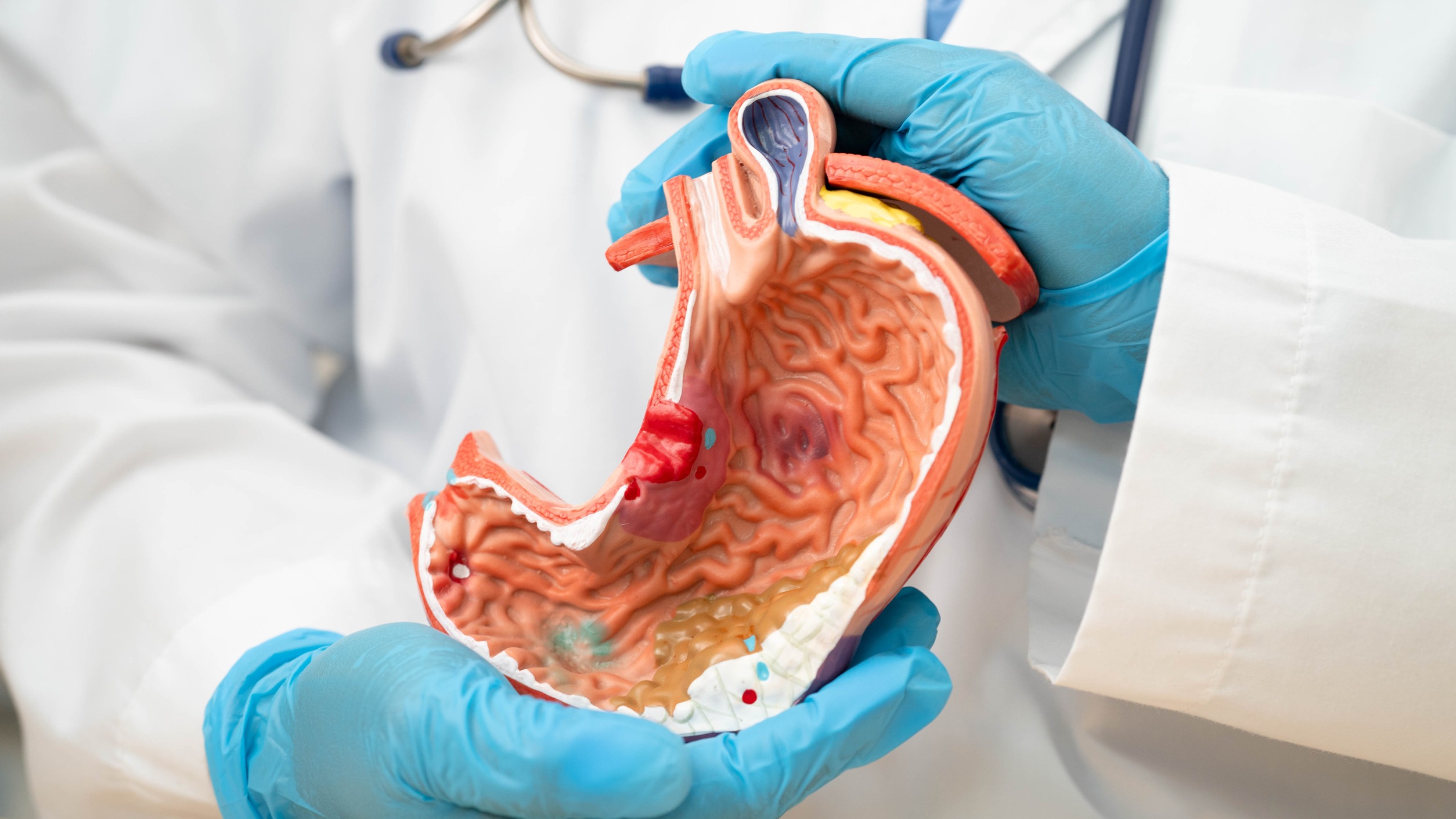
Understanding Gastric Cancer
Gastric cancer, a preventative cancer and a significant cause of death in at-risk populations, disproportionately affects various communities in the U.S. In particular, first-generation immigrants from regions with high incidences of gastric cancer are at elevated risk. Other groups include those with a family history of the disease and individuals suffering from specific hereditary GI polyposis syndromes.
Importance of Screening for High-Risk Groups
The latest AGA update emphasizes the importance of beginning screening in high-risk individuals. With robust evidence backing the use of endoscopic procedures, medical professionals can visually assess the gastric mucosa, identify areas of neoplasia, and perform biopsies when necessary. Dr. Doug Morgan from the University of Alabama highlights the integration of this screening process as essential to modern gastroenterology—comparing it to established practices used for colorectal and esophageal cancers.
Complementing Screening with H. Pylori Eradication
Yet screening is only part of the prevention strategy. The AGA guidelines stress the importance of eradicating Helicobacter pylori (H. pylori) as a critical component of gastric cancer prevention. This bacterium is known to increase the risk for gastric cancers, and proactive screening for H. pylori in high-risk populations can serve as a crucial early intervention. Studies suggest that this dual approach of screening paired with risk factor management can tremendously enhance outcomes and reduce deaths.
The Road Ahead: Future Predictions and Insights
The future of gastric cancer prevention cannot overlook the technological advancements in endoscopy. High-definition white light systems with image enhancement, proper mucosal cleansing, and adequate inspection time can make a significant difference in early detection. As these practices become standardized, we can foresee a decrease in mortality rates associated with gastric cancer.
Why This Matters: The Real-World Benefits
For suburban professionals aged 25-50—the target demographic for health innovation—being informed about gastric cancer risks can be a key aspect of taking charge of your health. The statistics are sobering: gastric cancer remains one of the deadliest cancers, but with proactive screening efforts, the landscape can change dramatically, reducing both incidence and mortality.
Common Misconceptions and Myths Around Gastric Health
Many people believe that cancer detection is predominantly focused on those who are older. However, age is merely a number, and gastric cancer can emerge much earlier, especially for those with genetic predispositions. Proactive care, rather than reactive treatments, empowers individuals to take charge of their health.
A Call to Action for the Health-Conscious
Navigating the waters of health and well-being requires an active approach. As we equip ourselves with knowledge from updates such as these, it is essential to consider being screened if you belong to a high-risk group. Consult with your healthcare provider about risk factors and the necessity for regular endoscopic examinations and H. pylori screening. Empowering yourself with this information can lead to better outcomes: your health is your wealth, and your prevention starts now.
 Add Row
Add Row  Add
Add 




Write A Comment