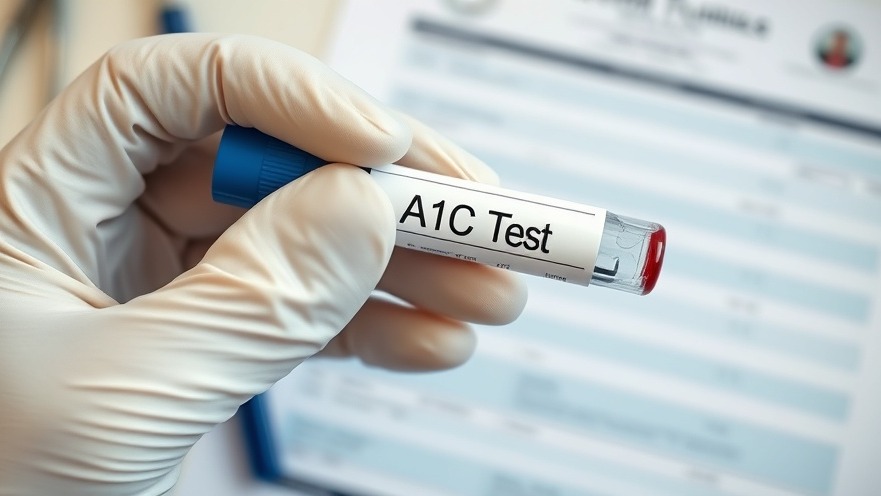
Improving A1c Testing: A Temporary Triumph or a Long-term Solution?
In a recent study led by Dr. Daniel L. Shaw and published in The Journal of Emergency Medicine, an intervention aimed at enhancing A1c testing among patients with diabetes revealed both promising successes and significant shortcomings. Conducted over several years, the research analyzed data from 348,490 emergency department (ED) visits. It found that implementing an alert system for overdue A1c tests notably boosted testing rates, but did not lead to substantial improvements in long-term glycemic control.
The Alert Implementation: Key Findings
Beginning in November 2017, healthcare providers employed an alert system specifically targeting 13,609 diabetic patients who had missed their routine biannual A1c tests. This proactive step led to a remarkable increase in compliance—from just 1.5% to a peak of 22.5% within the first year—demonstrating that strategic alerts can successfully prompt necessary screenings. However, this success was not sustained over time; by the sixth year following the intervention, compliance dropped to 5.1%.
Short-term Boost, Long-term Challenges
Despite the initial uptick in testing, the study revealed that only 15% of those who were noncompliant achieved their target A1c levels (< 7.0%), compared to 26% within the general ED population. The average A1c levels decreased insignificantly—from a decrease of -0.60 pre-intervention to -0.42 post-intervention—underscoring that this alert alone was not enough to ensure effective glycemic management after the immediate response wore off.
Patient Education: A Key Component
One critical takeaway from the research is the necessity of ongoing educational communication. As the alert system proved operationally feasible, the lack of consistent reinforcement messages contributed to the decline in A1c testing over time. Without reinforcing the importance of regular testing and overall diabetes management, patients may fall back into old habits of neglecting their health. Educational efforts alongside the alert may lead to improved outcomes.
The Bigger Picture: Reshaping Diabetes Care in Emergency Settings
This study highlights an essential aspect of chronic disease management within emergency care systems. While the initial response is encouraging, the challenge remains in building a sustainable plan that incorporates ongoing patient education and follow-up care. Incorporating these strategies could result in not only increased testing but also better long-term health outcomes.
Broader Implications for Diabetes Management
Looking forward, hospitals and healthcare systems could benefit from evaluating their diabetes management protocols. Integrating regular follow-ups and educational touchpoints can reinforce the importance of monitoring and help patients adjust their behaviors. With approximately 37 million Americans living with diabetes, as stated by the CDC, effective management strategies within ED settings are crucial in addressing the epidemic.
Conclusion: Encouraging Change for Better Health
In conclusion, while the emergency department alert system notably increased A1c testing, it also illuminated the gaps in ongoing patient engagement and education. For suburban professionals aged 25-50, understanding these dynamics can be critical for managing one's health proactively. Emphasizing the importance of regular testing and follow-ups ensures that patients can take charge of their well-being. Consider discussing your health goals with your healthcare provider today and explore strategies to enhance your health management. The journey towards better health begins with a single step, or in this case, a test!
 Add Row
Add Row  Add
Add 

 Add Row
Add Row  Add
Add 

Write A Comment